Report
Learn how PerfectServe's rules engine makes care team collaboration easier.
Read Now >>Patient care is only as strong as the clinicians who deliver it. Yet decisions about “fixing” burnout and workforce shortages are too often made without asking the very people living the problem every day. How do your clinicians experience the day-to-day of patient care and administrative burden? We wanted to find out, so we asked 343 clinicians to tell us what changes are really needed to reduce burnout, increase job satisfaction, and help them focus more on providing the best patient care. In this report, we bring forward the voices of clinicians themselves — what they say must change if we want them to stay in the profession and keep patient care at its highest standard.




– Nurse Practitioner at post-acute care facility (15+ years of clinical experience)
At the bottom of the list? Wellness programs and mental health resources.
What your clinicians need—and what they’re asking for—is for their leadership to address some of the most common gaps and problems that frequently undermine patient care and contribute to burnout.
As we’ll see in the results below, the problems clinicians are pointing out are all connected to your organization’s operational systems: unbalanced schedules, alert fatigue, and fragmented communication.
With insights pulled directly from nurses and doctors, this report highlights what clinical staff need to survive and thrive in their current roles. And for clinical leaders and health system executives, it offers a candid, necessary look at what your teams say they need from you.
Are you ready to listen?
Here are some of the standout insights from our survey of physicians and nurses:
Many clinicians cited a range of problems that stem from poor scheduling practices, including workload intensity (49%) and fatigue from prior days/weeks (38%)
Nearly three-fourths (72%) of clinicians must deal with a manual element to scheduling, increasing the risk factors that affect clinician well-being and quality of patient care
Over half (57%) of nurses and practitioners say waiting for calls/messages takes time away from patient care
6 out of 10 clinicians say current systems only sometimes, rarely, or never help prioritize urgency when dealing with high-stakes clinical situations
The message is clear: You have an experienced, passionate workforce asking for leadership to address the problems that increase their day-to-day stress and get in the way of patient care.

– Physician at a large hospital or academic medical center (8-15 years of experience)

– Registered Nurse at a mid-sized hospital or health system (4-7 years of experience)
Throughout this report, you’ll read insights from these experts:

Kelly Conklin
MSN, CENP
Chief Customer & Clinical
Officer, Former CNO

Miriam Halimi
JD, DNP, MBA, RN-BC
SVP of Client Services
Former CNIO

Simon Elliott
Director of
Customer Solutions
To understand the lived experience of today’s clinicians in the context of modern operational healthcare challenges, we partnered with independent research platform Centiment to survey nurses and physicians across 4 priority topics:
SCHEDULING AND WORKLOAD FAIRNESS
COMMUNICATION FRICTION AND ROUTING
PATIENT CARE AND OUTCOMES
LEADERSHIP, SUPPORT, AND CLINICIAN WELLNESS
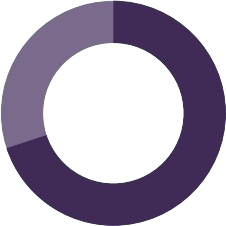
In the end, we collected responses from 343 nurses and physicians working across large hospitals or academic centers, mid-sized hospitals or health systems, community or rural hospitals, ambulatory/ outpatient care centers, and other care settings. Our collected feedback represents the views of an experienced, accomplished workforce: nearly 2/3 (64%) of respondents have at least 8 years of experience in healthcare, and 33% have been clinicians for 15 or more years. Here’s what those clinicians told us about the effects operational challenges are having on their well-being.
Physician (MD/DO)
45.2%
Registered Nurse (RN)
37.3%
Nurse Practitioner (NP)
7.9%
Advanced Practice Provider (APP)
5.2%
Clinical Supervisor or Charge Nurse
4.4%
Large hospital or academic medical center (500+ beds)
46.6%
Mid-size hospital or health system (100-499 beds)
26.8%
Community or rural hospital (<100 beds)
10.2%
Ambulatory/ outpatient care center
11.5%
Post-acute care (e.g., rehab, skilled nursing)
3.5%
Other
1.3%
15+ years
32.6%
8-15 years
31.6%
4-7 years
24%
1-3 years
11.2%
Less than 1 year
0.6%
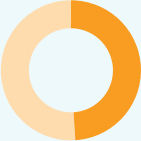
Most healthcare organizations continue to use scheduling systems that rely on a mix of basic scheduling portals and manual scheduling tasks. For many clinicians, this approach has “worked,” but the results aren’t great: 56% of nurses and practitioners said they experience regular spikes in demand or frequently feel overwhelmed and underresourced. Meanwhile, 31% describe their workload as manageable, while only 15% said they consider their schedule well-balanced.
WORKLOAD BALANCE ON A TYPICAL SHIFT
Manageable but with regular spikes in demand
Balanced and manageable for our staffing level
Frequently overwhelming; under-resourced
Varies too widely to generalize
I’m often under-utilized or assigned below my capacity
Providing all clinicians with a fair, balanced workload requires a scheduling system that can account for a wide range of complex rules, preferences, and other factors.
Even as many healthcare leaders attempt to address clinical burnout across their organizations, more than 85% of clinicians see at least 1 recurring issue with how their schedules are currently designed. Their top issues with current scheduling practices include:
Overall workload intensity: Nearly half of clinicians said their employer’s current scheduling system does not adequately consider patient census or acuity when assigning schedules.
Personal schedules and personal commitments: Failing to honor time-off requests and other personal scheduling needs can directly contribute to reduced job satisfaction and burnout.
Fatigue from the prior day or week of work: Clinicians expressed frustration over workload imbalances and exhaustion that can accumulate across shifts and contribute to burnout.
Patient continuity of care: Existing scheduling practices routinely overlook patient continuity of care when setting shifts and assigning clinicians. This can negatively impact patient transitions and overall clinical care.
FACTORS NOT ADEQUATELY CONSIDERED
IN HOW SCHEDULE IS BUILT
Workload intensity (acuity, census)
Fatigue from prior day or week
My personal schedule or personal commitments
Patient continuity of care
My individual preferences
Time-off benefits
Previous night/day transitions
None; I feel my schedule is well-balanced
Role or licensure-specific scope

– Clinical Supervisor at a mid sized hospital or health system (15+ years of experience)
In short, most healthcare organizations are still employing scheduling methods that rely on a mix of rudimentary tech and human oversight. Asking one or even multiple people to sort through so many layers of nuance as they attempt to account for each of these factors is a recipe for mistakes and suboptimal schedules.
“When you’re manually scheduling, you can have as many intentions as you want,” says Simon Elliott, Director of Customer Solutions at PerfectServe. “As a human building the schedule manually, sometimes it’s hard to find a schedule that’s going to allow you to try to strike that perfect balance for your team without compromising what you need from an operational perspective.”
Auto-generated schedules are a potential solution to these challenges, especially when scheduling tech can account for a wide range of advanced rules to create schedules that are optimized both for individual clinicians and the needs of the larger care team. But most clinicians don’t have access to those tools: 7 out of 10 clinicians said their healthcare organization’s scheduling process involves manual elements that contribute to a number of pervasive problems, including unbalanced workloads and a perceived lack of fairness when clinicians’ requests or preferences are not regularly honored by the scheduler.
This is where technology and automation can make a night-and-day difference for scheduling. Some automated staff scheduling software can account for complex rules specific to shift spacing, scheduling equity, and clinicians’ personal requests to build workloads without the gaps and oversights that are inevitable with manual scheduling.
of clinicians said their healthcare organization’s scheduling process involves manual elements that contribute to a number of pervasive problems
Auto-generated scheduling can also adapt to the needs of your patient population, allowing your organization to more flexibly adapt to changes in patient census and acuity while maintaining consistent patient-clinician relationships for better continuity of care. But creating a truly effective schedule isn’t only about matching physicians and nurses to patient ratios—it also requires understanding the mix of supporting staff needed to care for the patient population present during each shift.
“There’s been a lot of talk over the years about looking at patient census and provider workload based on the acuity or severity of the patient,” says Kelly Conklin, a former CNO who now serves as Chief Customer Officer and Chief Clinical Officer at PerfectServe. “Those are all important considerations, but they’re focused on the nurse-to-patient ratio. When you’re talking about bedside nursing, the bigger issue is the number of supporting staff that are assigned to care for a given patient population on the same shift.”
– Physician at a mid-sized hospital or health system (4-7 years of experience)
Clinicians told a complex story about the communication systems their organizations use. Their insights illustrate how easy it is to overlook the consequences of fragmented communication. For example: 87% of clinicians cited at least 1 point of friction that routinely complicates communication during their shift. The top factors include:

Delays in call and message replies, which create a slowdown effect during any shift

Reaching providers unfamiliar with the case, often resulting from inaccurate call schedules and improper routing

Communication relayed through third parties, increasing the risk of miscommunication and increasing the time spent waiting for a reply

Using too many different communication tools, creating confusion and inefficiency when trying to send the right message to the right person
FACTORS THAT SLOW DOWN OR COMPLICATE
COMMUNICATION DURING SHIFTS
Delays in call/message responses
Communication relayed through third parties
Reaching providers unfamiliar with the case
Using too many different devices/platforms
No escalation process when someone is unreachable
Not knowing who’s on call
None of the above
From a functional point of view, things might appear to be going okay: While only 27% of clinicians communicate through a unified platform—meaning 1 platform for all types of communication—nearly 1/3 still rely on their personal device, and almost 2 out of 10 still use a pager.
COMMUNICATION ENVIRONMENT
Multiple tools for different message types
I use a personal device for work communications
Communication includes EHR integration
Devices vary by shift or department
Escalation protocols built into communication
Unified messaging in one platform
I still use a pager
There’s no consistent system across my unit
At the same time, 7 out of 10 clinicians use at least 3 tools for day-to-day communication, with 16% using 5 or more. When we talk about app fatigue, this is a prime example.
NUMBER OF DIFFERENT PLATFORMS OR
APPS USED ON A TYPICAL SHIFT
1-2
3-5
5-6
7 or more
Unsure
Clearly, technology and communication systems are often a source of stress for clinicians, rather than being the helpful tools they’re meant to be. The top changes clinicians said would reduce daily stress in their roles include:

More staff for critical times, underscoring the impact imbalanced schedules and workloads can have on clinician wellness
Clearer communication workflows, such as fewer communication channels, less difficulty reaching the right on-call providers, and auto-escalations to ensure critical messages always get the attention they need
Less administrative burden, such as redundant paperwork and added time spent triaging messages
FACTORS THAT WOULD HELP
REDUCE DAY-TO-DAY STRESS
More staff for critical times
Clearer communication workflows
Less administrative burden
More predictable and fair scheduling
Fewer systems/devices to manage
Real-time shift/task load transparency
Improved leadership awareness of our daily reality
Access to wellness or peer support resources
Greater say in operational decisions
Coaching on facing negative patient outcomes
Relatively few clinicians cited communication errors or other challenges that occur frequently or on a daily basis. 26% cited receiving duplicate messages as a frequent or daily issue, while 24% said they routinely deal with messages that go unread or unacknowledged by their recipient. But 51% say they sometimes, often, or daily receive messages that are too late to act on. In a healthcare setting, “too late to act on” can very easily translate to negative consequences for patients.
On the surface, it might appear that existing healthcare communication systems are succeeding more than they’re failing. But when you extrapolate these error rates across tens or hundreds of thousands of communication events taking place in a 500-bed hospital every week, these shortcomings become an obvious source of inefficiency and chaos that can undermine operations and patient care.
All of these gaps in communication lead to a less effective system. At least 1/3 of clinicians have their doubts about the effectiveness of patient transitions between departments, to family members, and with care coordinators. Even more telling, only 55% of clinicians say current communication with ambulatory and outpatient staff is effective.

– Physician at a mid-sized hospital or health system (4-7 years of experience)
Fragmented communication isn’t only bad for your clinicians. It’s bad for patients, too.
“When we communicate in multiple modalities, it creates gaps in knowledge and shared understanding among the team,” says Kelly. “And when you think about high reliability as a science, it is that common understanding that gets us to the high reliability mark. When we have those gaps or we have those pathways that don’t lead back to the patient and the team that’s caring for them, that’s when harm happens.”
Fragmented communication can contribute to all kinds of mistakes and delays that cause unnecessary stress and harm to patients. Maybe critical lab results are slow to reach the appropriate person because they’re initially sent to a physician who isn’t working. Or perhaps incomplete communication between outpatient and emergency care facilities causes critical information to become lost during a patient transition.
Kelly recalls a particularly egregious story where a pathology report was sent to a cancer patient first, giving them time to misinterpret its findings since they had no guidance from their physician.
“They went ahead and read the report with layman’s terms,” Kelly says. “And they were certain their cancer was worsening. They went ahead and told their family. Then 5 hours later, the physician calls and says, ‘So sorry for your misunderstanding, but actually, your tumor is shrinking.’”
In critical care situations, the consequences of fragmented communication become even more glaring. When time-sensitive updates or issues arise during a shift, only 46% of clinicians are very confident that they can reach the right person, and just 38% say their current clinical communication system consistently allows them to prioritize messages.

– Physician at a large hospital or academic medical center (15+ years of experience)
ABILITY OF CURRENT SYSTEMS TO PRIORITIZE
URGENT VS. NON-URGENT MESSAGES
Yes, consistently
Sometimes
Rarely
No, not at all
CONFIDENCE IN REACHING THE RIGHT PERSON
FOR URGENT UPDATES DURING A SHIFT
Very confident
Somewhat confident
Not very confident
Rarely confident
It depends on the type of issue
During a recent site visit to a hospital, PerfectServe SVP of Client Services Miriam Halimi—who once held the role of CNIO at a large health system—saw firsthand how the slowdown created by fragmented communication can have downstream effects on patient care. According to Miriam, the hospital’s call schedule system and communication system weren’t integrated with one another, which means users had to log in to the call system to see who was on call before sending a message to the appropriate clinician.
“When I think about routing, it’s so critical to have the right provider call schedules,” she says. “Communication often starts with who’s on call. That’s one of the biggest routing issues that we run into, is when we don’t have the right call provider, or it’s not updated correctly, and then it’s routed to the wrong person. And care can be delayed!”
Communication and scheduling gaps have direct implications for patient care. But the specific ways they undermine patient care are diverse, which highlights the need for systemic change rather than band-aid fixes to acute operational issues. Case in point: nearly all clinicians surveyed (96%) identified at least 1 issue that regularly took time away from direct patient care. The most commonly cited issues include:
Waiting for call-backs or responses to messages, which can pose a significant risk to patients when those delays interfere with providing direct care in an urgent situation.
Dealing with non-clinical administrative tasks, which pulls them away from working at the top of their license and takes up time that could be spent on patient care.
Logging into multiple systems/devices, which slows down communication and forces clinicians to navigate information gaps on their own
(e.g., logging into separate platforms to check the on-call schedule and send a message instead of doing both in one interface)
Repeating documentation across multiple systems, a task made necessary when communication and charting tools don’t share information—forces clinicians to spend valuable time re-entering the same details instead of caring for patients.
TASKS THAT REGULARLY TAKE TIME AWAY
FROM DIRECT PATIENT CARE
Waiting for call-backs or responses
Logging into multiple systems/devices
Non-clinical administrative tasks
Repeating documentation across platforms
Alert fatigue from unnecessary notifications
Searching for contact info or role coverage
Training on new systems or updates
Redundant or unclear messages
Family updates or coordination tasks
None of the above
It’s worth noting that many of the top factors affecting patient care also rank among the top factors contributing to clinician stress—illustrating the high priority clinicians place on providing the best direct patient care possible.

– Registered Nurse at a large hospital or academic medical center (4-7 years of experience)
Patient transitions offer another prime example of how communication gaps and friction points can hold clinicians back from providing the best patient care possible. 87% of clinicians said they regularly experience confusion or friction during patient transitions. The four most common responses include:
Delayed or incomplete documentation: Many clinicians expressed difficulty communicating with ambulatory and outpatient facilities, and these struggles directly affect patient transitions. Delayed, incomplete, and inaccurate information can directly impact continuity of care
Lack of ownership of handoff: Clear transitions and accountability are vital to continuity of care, and to verifying that all appropriate information and documentation is shared between providers
Unclear or missing contact information: From contacting past providers to reaching out to family members, inaccurate contact information forces clinicians to spend more time chasing information that may be critical to patient care
Uncertainty about roles and responsibilities: A lack of role clarity in transitions can lead to certain tasks and responsibilities falling through the cracks—contributing to missing documentation, delayed care, and a range of other errors impacting continuity of care
FACTORS THAT OFTEN CREATE FRICTION
OR CONFUSION DURING TRANSITIONS
Delayed or incomplete documentation
Unclear or missing contact information
Lack of ownership of handoff
Uncertainty about roles/responsibilities
Language or cultural barriers
Technology access or platform issues
Inadequate communication training
Nothing – transitions are smooth
Many of these challenges can be addressed with technology that drives operational change to mitigate the confusion and friction that stops clinicians from spending more time on direct patient care.
A clinical communication platform with advanced routing capabilities is one example. By building intelligence into routing that considers variables like time, day, urgency, service line, and on-call schedule, platforms like these remove the guesswork from communication and ensure that, regardless of the clinical scenario, that time-sensitive message will be delivered to the right person. This also allows for auto-escalation of messages that aren’t opened and answered in a timely manner, which drives more efficient communication and allows clinicians to focus on other work without worrying that they’re neglecting patients.
On the other hand, standardized alert tones and routing can reduce alert fatigue and make it easier for clinicians to triage which messages and tasks are their responsibility. “In PerfectServe, for example, clinicians get the same alerts, the same tones, and the same routing based on their organization’s standards,” Miriam says. “It takes the guesswork out of hearing an alert on the phone and thinking, ‘What does that tone mean?’ And that lowers the risk of missing an alert.”
Clinicians see a direct correlation between the non-clinical work they’re asked to do and the amount of time they’re able to spend on patient safety and care. By addressing the white noise, the surfeit of paperwork, and delays in back-and-forth communication, healthcare leaders can better utilize clinicians on the most urgent work affecting patient outcomes.

– Physician at a large hospital or academic medical center (15+ years of experience)
What clinicians are asking for is simple:
They want to be supported by leadership and equipped with tools and processes that allow them to focus primarily on patient care.
They want equitable scheduling to help them avoid burnout.
They want to be involved in the technology investments and operational changes aimed at improving clinical operations.
Why?
Because they’re working on the front lines of patient care, and they’re intimately familiar with the day-to-day friction caused by bad decisions, bad processes, and bad technology—the kind of friction that can adversely affect provider satisfaction and patient outcomes.
RANKING OF REASONS TO STAY
IN ROLE OVER THE NEXT 2–3 YEARS
(Excluding Pay)
Stronger communication and support from leadership
Predictable and equitable scheduling
Reduced non-clinical administrative work
Clearer daily workflows and expectations
More autonomy or input into decisions
Simpler technology systems
Wellness or mental health resources
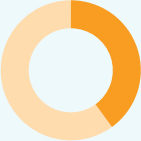
Whether leadership is listening to clinicians is a different story. In the last 12 months, only 33% of clinicians said their leaders made changes to the organization’s operational tools and workflows after soliciting feedback from clinicians. Meanwhile, 22% said their feedback didn’t result in any changes—and nearly 40% said leadership never asked for their input.
FEEDBACK REQUESTS ON OPERATIONAL
TOOLS AND WORKFLOWS
In the Last 12 Months
No, I have not been asked
Yes, and changes were made based on feedback
Yes, but no action was taken
I’m not sure

– Physician at a community or rural (15+ years of experience)
Does this mean healthcare leadership should feel compelled to act on every piece of feedback? Kelly says no.
“Sometimes the response is, ‘We’re not going to be able to do anything about what you brought up,’” she says. “Hearing ‘no’ is okay in most scenarios as long as clinicians understand the ‘why’ behind it. But no response whatsoever means you don’t value me.”
When operational systems show process limitations or inefficiencies, clinicians are asked to bridge the gap. But that added responsibility comes at a price: Clinicians inevitably end up feeling overworked, poorly utilized, and underappreciated by their leadership.
“When we begin to problem-solve and troubleshoot together, you’re always going to come up with a better solution,” Kelly says. “It goes back to hearing and listening to the voices of the clinicians. Some of the organizations that have the strongest cultures in place—the strongest nurse retention, the lowest vacancy rates—are those that give the voice and the power to those who do the work.”
As a basic standard, healthcare organizations should always save a seat at the decision-making table for the people impacted most by operational issues and potential technology changes.
– Registered Nurse at a large hospital or academic medical center (15+ years of experience)
Kelly, Simon, and Miriam point to a handful of tactics healthcare leaders can use to better prioritize communication with clinicians in the coming year:
As a healthcare leader, you could propose any number of targeted changes aimed at reducing clinician burnout, improving recruiting and retention, and/or better supporting patient care. But a piecemeal approach isn’t going to deliver the lasting impact you’re after.
It may seem like clinicians are voicing a bunch of different problems pointed in a bunch of different directions. And in your leadership role, you might be inclined to think that each problem can be fixed with a simple, targeted solution.
They’re all symptoms of deeper issues— imbalanced scheduling, inefficient communication, fragmented or broken workflows, and other process flaws in patient care—that are baked into your organization’s day-to-day operations.
To improve clinical staff wellness, you need to start with operational wellness. That’s our view at PerfectServe—and it’s why our
platform is focused on mitigating the root causes of clinician fatigue and burnout to yield:

Our team has worked with tens of thousands of healthcare organizations and hundreds of thousands of clinicians, and the focus has always been the same: Make critical healthcare operational systems better. This is why clinics, medical groups, and hospitals partner with PerfectServe. They want to move from point solutions to a unified platform that addresses many of the challenges clinicians are desperate to solve.
It’s not just about the technology, either: from CNO to floor manager, the PerfectServe team has direct experience within hospital and healthcare settings. That means our implementation and customer service teams know the right questions to ask to help you focus on operational wellness.
Talk to your internal leaders and tech specialists about how PerfectServe can help fix what’s broken in your clinical operations.