Report
Learn how PerfectServe's rules engine makes care team collaboration easier.
Read Now >>TABLE OF CONTENTS
Despite increased awareness and intervention efforts, nurse burnout remains a problem across most healthcare settings. This guide examines the hidden causes of the nurse retention crisis and provides nursing leaders with evidence-based strategies to combat burnout, improve retention rates, and create healthier work environments.
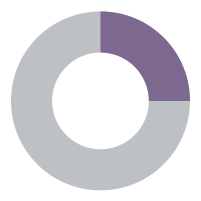
of all nurses report frequent burnout.
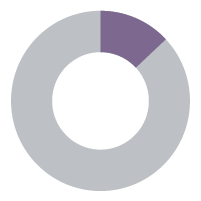
consider leaving their positions.

Nurses represent the front line of healthcare, touching nearly every step of a patient’s care journey. From the bedside to the operating table, their work is essential.
But the profession is facing an ongoing retention crisis. Nurses entered the field to care for people, but too often they’re forced to battle administrative tasks, complex technology, and safety concerns that keep them from doing what they do best.
Today, half of US healthcare workers, including nurses, report frequent burnout.1 While some pressures have eased since the pandemic, many of the triggers for burnout and turnover are not improving.
Staying late to chart. Missing breaks. Juggling unsafe patient loads. Enduring harassment or even violence. And the technology that’s supposed to help? It often makes things worse: more alerts, more alarms, more systems to manage.
The impact of burnout and turnover goes far beyond individual well-being. When experienced nurses leave, the ripple effects are immediate: heavier workloads for remaining nurses, longer onboarding for new hires, less collective experience to draw from, rising costs, and compromised patient outcomes.
So why the crisis? Nurses are overwhelmed. They’re tired. Their voices aren’t heard enough when people ask how to make things better. They don’t always feel valued. Too many are working their shifts in a fog, and change is long overdue.
Despite the magnitude of the problem, you can take some clear steps to improve the working environment for nurses.

—Danielle Jenkins, MBA, RN, BSN, CRNI
“The Nursing Staffing Crisis: Advocating for Safe Workplaces and Better Patient Care”
The pressure nurses feel starts with staffing. With more nurses leaving the field, those who remain are feeling the strain. They’re taking on more patients, doing more admin work, and sacrificing work-life balance to fill in the gaps.
of nurses cite staffing shortages as contributing to burnout in their current role.2
of US nurses say they feel burned out most days, based on a 2025 survey with more than 12,000 respondents.3
of nurses say they are somewhat or very likely to look for a new job.1
Staffing is only one piece of the burnout puzzle. Many health systems try to boost nurse satisfaction with “better” technology—new devices or automated shift updates. But without careful implementation, these well-intentioned fixes often add complexity and clutter, making workflows even more frustrating.
of nurses report that a chaotic work environment contributes to burnout levels.4
of nurses have little to no say in their shifts or schedules.5
of nurses report that EHRs inhibit efficiency and contribute to burnout levels.4
It’s important to note that burnout isn’t just an ephemeral metric. The average cost of turnover for a staff nurse is just north of $61,000, and for each percentage point change in nurse turnover, the average hospital will either save (if nurse turnover goes down) or lose (if nurse turnover goes up) roughly $289,000. In an environment where the average acute care hospital loses about $4.75 million annually, these figures are especially important.
The average cost of turnover for a staff RN, with a range of $49,000 to $72,000.6
The average acute care hospital lost $4.75M in 2024, with a range of about $3.85 to $5.65M.6
Each percent change in RN turnover stands to cost or save the average hospital $289,000 per year.7


– 2025 NSI National Health Care Retention & RN Staffing Report6
Staffing ratios are a central part of the discussion when it comes to preventing burnout and maintaining safe patient care. In 2025, only a handful of states have laws that set minimum nurse-to-patient ratios, while most leave staffing decisions up to hospitals. This often leads to heavier workloads, especially as hospitals struggle to fill vacant positions.
The nursing shortage has unfortunately—and perhaps understandably— contributed to an increase in medical errors. A 2025 survey found “54% of nurses reported being aware of medical errors occurring due to unsafe nurse staffing levels,” and “26% of RNs said they’ve witnessed patient deaths that they believe are linked to unsafe staffing.”8
Without consistent safeguards, nurses are stretched far too thin, increasing stress, fatigue, and the risk of burnout while also impacting the quality of care patients receive. Data reveals just how much:
Modern nursing requires extensive documentation and compliance activities. While some of these tasks are necessary, they keep nurses from working at the top of their license and limit the time available for patient care.
Many nurses stay after their shifts to complete charting, creating a nurse equivalent of “pajama time” that leads to work-life balance issues and potential disciplinary action for late documentation or even taking too much overtime.

Kelly Conklin
Chief Customer & Clinical Officer, PerfectServe

Too often, health systems have layered on platform after platform in the name of efficiency. But instead of simplifying workflows, nurses are left juggling multiple logins, alerts, and dashboards—each demanding attention but rarely working together.
For example, a nurse may receive lab results in the EHR, a secure message from a physician in a separate app, and an urgent page through yet another alert system. If none of these tools “speak” to each other, the nurse has to stop, check multiple platforms, and often re-enter the same information in multiple places just to complete basic tasks.
The impact is staggering. A time-motion study found that nurses can spend more than a third of their working hours (34%) just managing communication across multiple platforms.11 Instead of reducing friction, technology bloat—along with poor integration—has become one of the main forces driving burnout.


Kelly Conklin
Chief Customer & Clinical Officer, PerfectServe

As a result, by the time a patient ends up in the hospital, they’re often much sicker than they would have been 10 years ago. Even if a nurse’s patient load hasn’t necessarily increased, today’s patients typically require more time, care, and attention. This means nurses have less time for everything else, like charting, taking a break, sending updates or follow-ups to patients and their caregivers, or checking in with their team.
Over time, that constant pressure builds up. Even if the number of patients stays the same, the workload doesn’t just feel heavier—it is heavier.
Many health systems still rely on hours per patient day (HPPD) calculations for scheduling, but these don’t account for patient complexity or acuity levels. This mismatch between scheduled time and actual workload creates chronic understaffing situations.
On top of scheduling workflows that aren’t optimized for breaks and administrative time, outdated physician scheduling workflows make even simple tasks unnecessarily difficult. Imagine a nurse trying to escalate an urgent patient concern. The on-call schedule is outdated or buried in a separate system, so he spends valuable time trying to find the right provider. When he finally makes a call, he reaches the wrong provider because the on-call doc listed on the schedule had changed and wasn’t updated.
Now, our nurse has to start over, which wastes minutes he doesn’t have, delays care, and adds another layer of frustration to an already overloaded shift.
On top of excessive patient load and administrative tasks, care team members face untenable levels of workplace violence.
These numbers are frightening statistics—but they aren’t unfixable.
Creating safer environments requires both cultural change and smart technology. Many health systems have seen success with emergency alert protocols (think Code Violet or Code Green), which allow nurses to discreetly alert security about an agitated patient or family member, often through an existing communication platform. The earlier the signal, the sooner the response, and the greater the chance of de-escalation.
This requires a modern alert system that can get these notifications to the right personnel in a timely manner. Personnel who arrive to address the situation must also be able to decipher this type of alert from other situations, like an active shooter or severe weather. Clear, differentiated signaling ensures the right response at the right time.
1 in 4 nurses experience workplace violence.12
of missed workdays are attributable to workplace violence incidents.12
of workplace violence
incidents are reported.12

Kelly Conklin
Chief Customer & Clinical Officer, PerfectServe

Nurses typically field a large number of calls, messages, alarms, and overhead pages. While most alerts don’t require immediate action, they still interrupt workflows, fuel alarm fatigue, and pull nurses away from the bedside.
Poor communication with providers makes these challenges even worse. Nurses routinely struggle to communicate quickly and efficiently with providers due to out-of-date provider schedules, slow response times, rudimentary technology, and the many other routine events that limit provider availability throughout the day.
Effective communication systems can change this by:
Clear communication channels and reliable message routing can prevent some of the frustration and delays that contribute to burnout. Neither nurses nor any other care team member should have to guess who’s on call or whether their messages are being read.
REAL-WORLD SCENARIO
A patient’s condition slowly worsens, but the nurse can’t reach the on-call physician. Messages go unanswered with no delivery confirmation. The situation becomes urgent, forcing the nurse to call a code per hospital procedure. When the physician finally arrives, he lectures the nurse in front of his colleagues because he didn’t understand how a routine matter got out of hand—even though his own unresponsiveness was the primary cause.
The reality? In this instance, the nurse was actually punished for doing her job correctly
To avoid situations like these, hospitals aren’t just turning to better communication tools. They’re looking at unified collaboration solutions that span all locations & care team members and provide real-time schedule visibility to ensure all messages are delivered to the right recipient in a timely manner.
Other benefits of modern care team collaboration software:
KLAS Research found that 65% of nurses cite staffing shortages as a driver of burnout.4 But the problem goes beyond the number of nurses a hospital employs. A 2024 Washington Center for Nursing study found only 58% of staff nurses can participate in developing their schedules.13
Feeling like you have no control over your schedule is also strongly correlated with burnout. But many hospital scheduling systems are so inflexible that individual needs and preferences are seldom taken into account. In some cases, nurses are assigned more patients than they can reasonably care for, and others are overscheduled to the point where even short breaks aren’t feasible.
Simply “buying better tech” won’t fix this. Real progress requires smarter staffing models that address shortages proactively, more flexible scheduling, and clearer communication that gives nurses greater control over their day-to-day work.
Nurses are the largest segment of the healthcare workforce, but somehow, they’re seldom consulted on major IT decisions. Make that make sense.
These are the people charting vitals, tracking meds, and coordinating care—the ones who use the technology the most. And yet, their voices are often missing from the conversations that shape their daily workflows.
Why? Often out of a misguided sense of protectiveness. Amanda Brown, VP of Nursing Workforce Optimization at Baptist Health, says there’s often an attitude of, “Let’s not worry the nurses with this. Let them take care of the patients.” Nurse managers, in particular, are seen as already stretched thin, so instead of being invited into the process, they’re shielded from it.

Amanda Brown
VP of Nursing Workforce Optimization, Baptist Health

Despite these seemingly good intentions, this kind of thinking does more harm than good. Rather than protecting nurses, leaving them out of discussions means they’re more likely to end up with tools that make their lives harder.
Finding ways to include nurses in the tech decision-making process is the best way to increase adoption and ensure their buy-in. Not to mention, nurses who feel heard and valued are far more likely to stay with their organization.
When nurses are included in larger decision-making processes, organizations can expect to:
Embedding the clinical communication platform within the EHR led to a
increase in nurse satisfaction and a
bump in messaging use YoY.

Building nurse feedback into tech decisions doesn’t have to be complicated, but it does have to be intentional. Nurses are busy, practical, and deeply aware of how technology shapes their daily workflows. If you want their input to be meaningful (and their adoption to be successful), you need a clear framework.
That’s where SCRUB comes in. Just like nurses scrub in before every procedure, leaders can SCRUB into their tech decision-making process to ensure nurse feedback is built in from the start.
S
Simplify Participation: Nurses have demanding schedules, so make it easy for them to show up. Send online invites and schedule meetings at workable times. Include brief summaries about the need to discuss upcoming tech changes so participation feels manageable and not like an extra burden.
C
Clarify Roles: Nurses aren’t sitting in meetings all day—they need clear framing. Lay out the problem, explain why a new tool or process is being considered, and outline realistic options. When expectations are transparent, feedback is more focused and actionable.
R
Real Choices Only: Nothing disengages nurses faster than being asked to weigh in on decisions that aren’t actually theirs to make. Bring them options they can actually influence, and save the “someday” conversations for later.
U
Understand Cost: Don’t shy away from budget discussions. Nurses are practical, and when they see the trade-offs, they’ll help choose the option with the U greatest impact on patient care. Transparency builds trust and smarter decisions.
B
Build Feedback Loops: Not every nurse will feel comfortable speaking up in a big meeting. Offer multiple ways to give input—polls, forms, quick one-on-one conversations—so every voice can be heard.
SUCCESS STORY
At MemorialCare Orange Coast Medical Center, nurses were frustrated with outdated communication processes. Reaching the right provider often meant chasing down schedules, waiting on callbacks, or relying on noisy overhead pages. Delays were common, workflows were messy, and nurses felt the strain. When the hospital implemented a clinical communication platform with intelligent routing, communication improved dramatically. Nurses could connect directly with the right provider without hunting down schedules or sending pages through intermediaries. This meant faster responses, less noise, and a smoother workflow that gave time back to the bedside.

Impact on Nurses
Clinical & Operational Outcomes

By reading this guide and considering how to improve the lives of your nurses, you’re already taking the first step.
That step means shifting the conversation from simply acknowledging that “burnout is a problem” to actively asking, “How do we support well-being?” The real burnout trigger isn’t just stress, but stress that feels unnecessary, unfair, and unrelenting. It’s the experience of being overworked and overscheduled, the burden of inefficient communication, and the juggling of multiple systems just to accomplish simple tasks.
By addressing the biggest and most consistent challenges nurses face every day—and helping them feel valued and safe at work—healthcare organizations can mitigate the stress contributing to burnout, improve nurse retention, and empower nursing staff to provide even better patient care.
Recommended next steps:
Ready to make lasting changes?
We’re here to support you. If you have any questions about this guide or want to learn more about how PerfectServe’s solutions can make work easier for nurses, reach out today!