Getting Your Care Team On One Unified Platform
Call Center, Clinical Communication and Collaboration, Hospitals and Health Systems, Medical Answering Service, Patient & Family Communication, Provider Scheduling,
TABLE OF CONTENTS

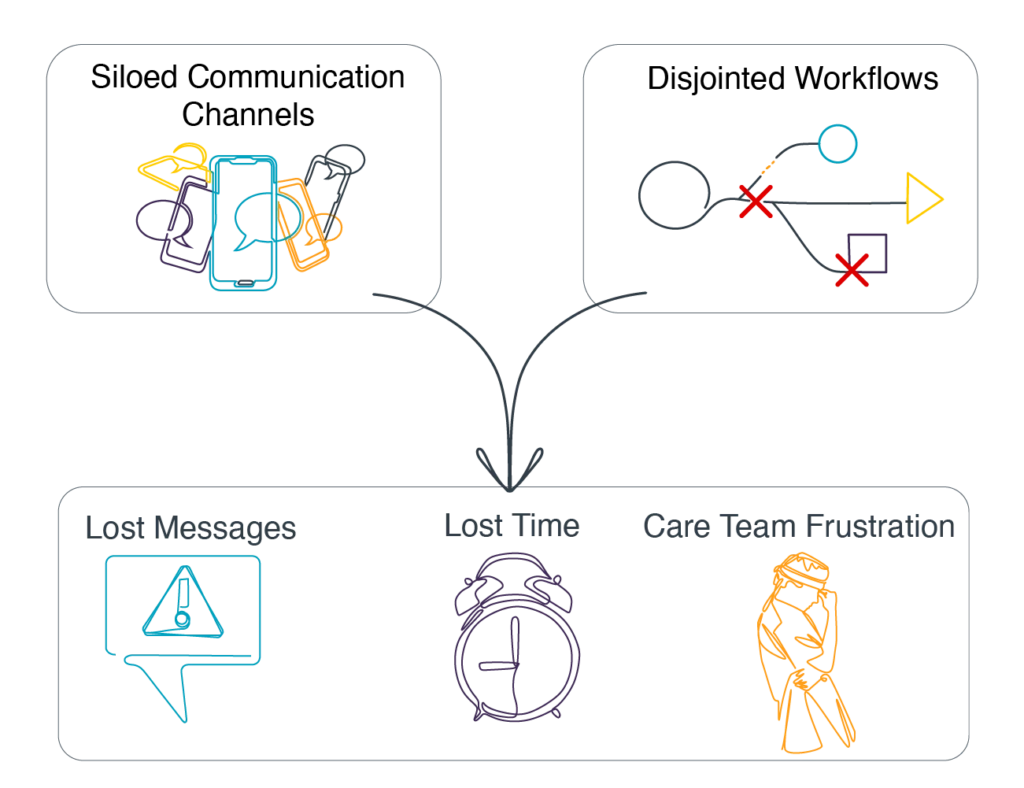
Inefficient clinical communication workflows can negatively impact both patient safety and provider satisfaction. A few factors in particular contribute to suboptimal communication within the care team:
- Siloed communication channels: Many organizations still use multiple communication channels to coordinate patient care. When clinicians have to jump from app to app to communicate, it’s difficult to coordinate care efficiently, and the risk of making mistakes increases.
- Disjointed workflows: Maybe it’s difficult for clinicians to find the right colleague to connect with for a given patient scenario, or perhaps an organization is using EHR-based secure messaging that lacks proper routing and escalation capabilities. Either way, disjointed communication workflows can lead to treatment delays, extended lengths of stay, unsatisfied patients, and an elevated risk for patient harm.
The above factors can lead to various downstream challenges, including:
- Lost messages: When communication methods lack sophisticated routing capabilities, the risk of “losing” them increases significantly, especially if a critical message goes to the wrong person or lands in a generic inbox that isn’t monitored in real time.
- Lost time: If nurses and other care team members waste valuable time tracking down physicians to share or retrieve information, the resulting frustration contributes to higher levels of burnout and reduces direct patient care time.
- Care team frustration: The frustration that stems from disjointed workflows and siloed communication channels can contribute to elevated care team burnout, which makes it harder to provide patient care of the highest quality.
How to Unify Clinical Communication
These challenges can be mitigated with technology that is designed from the start with enterprise communication in mind. Whether it’s a critical access facility or a multi-site health system, a unified healthcare communication and scheduling platform can improve patient care, enhance provider satisfaction, reduce costs, streamline important clinical workflows, and give time back to the entire care team.
Moving from multiple solutions to one platform—part of a trend called “vendor consolidation” that’s picking up steam in the industry—can also help healthcare organizations develop more meaningful vendor partnerships. Rather than working with five vendors on five different aspects of your communication infrastructure, why not forge a long-term relationship with one vendor who can support every part of your strategy? This can lead to more effective collaboration, deeper understanding, and better results.
But that’s just a primer—it’s time to dive into details. What should you keep in mind when considering an all-in-one healthcare communication and scheduling platform?
Effective Communication Requires a Good Schedule
Ineffective scheduling practices are often at the root of poor communication. Think about it—if the care team is constantly forced to reference the EHR, whiteboards, binders, intranet sites, and phone lists, how can they be expected to contact the correct care team member in a timely manner every time? Time is wasted when they have to search, check, and re-check. And when a critical lab result comes in, how long is too long before the correct attending physician knows it’s ready?
This isn’t anyone’s fault, and everyone is doing their best. But to facilitate the kind of efficient communication that makes real-time patient care possible, it needs to be much easier to create and distribute consistently up-to-date schedules. You can do this by aligning your care team on one scheduling platform that auto-generates optimized schedules, accommodates provider preferences, updates in real time, and is accessible from any location via desktop or mobile app. Communication workflows should be directly influenced by the schedule to make sure the right people are always on the receiving end of messages, calls, and alerts.
In short, good schedules and effective clinical communication go hand in hand.
Getting Messages to the Right Provider at the Right Time
Now that the schedule is accurate, it’s easier to get messages to the right provider. Routing built on accurate schedules can account for variables like time, day, urgency, service line, and contact preferences, so when a message is sent, it’s delivered accurately regardless of circumstance or urgency. No more lost messages, and no more guessing if a message was delivered or read. No matter who’s scheduled, who’s available, or how the schedule might have changed, all communications are instantly delivered to someone who’s able to respond and take action.
As an additional benefit, by having all of these messaging workflows within one intelligent platform, certain metrics—such as the time it takes for a message to be read and responded to—can be monitored over time. This capability gives insight into areas in need of improvement.
Your Communication Ecosystem Should Include the Operator Console
Hospital operators can be heavily impacted by disjointed communication workflows. As the “hubs” for all things communication throughout the hospital, call/transfer/command centers need an interface that allows operators to seamlessly route inbound calls from patients and providers to the right place. With an operator console that lives within your communication platform and is integrated with real-time staff and provider schedules, you can make life easier for operators, enhance call and message routing for the entire care team, and protect patient satisfaction.
Inbound calls that aren’t handled efficiently—whether they’re coming from patients or a referring provider—can easily cause frustration, and the caller may choose to contact a competing hospital. An operator console that lives within your clinical communication platform can solve this problem. For example, if an operator has the on-call schedule open within the console and receives a call requesting to speak to someone in the ED, they can easily search for and contact the “ED physician on call.” The operator can then transfer the call with a few clicks, and the caller is quickly connected to the right provider. Gone are the days of paper schedules and the often-ineffective “page and pray” technique.
Don’t Overlook the Answering Service
Some people think of the answering service as nothing more than a cost center, but it’s an important connection point that shouldn’t be overlooked. The main challenge that healthcare organizations experience with answering services is that they depend too much on poorly trained and unreliable live agents. These agents can’t keep up with who’s on call, and often manually route messages to the wrong person. This is why integrating real-time schedules with the answering service is important—it reduces unnecessary interruptions, especially after hours.
Smart communication workflows can just as easily be applied to a small private practice as they can to a larger facility like an academic medical center. By building your answering service functionality into the same intelligent, cloud-based communication platform used by the rest of your staff, you can ensure that all off-hours calls—whether urgent or routine—are handled appropriately. This is a satisfier for patients and providers alike.
Make Patient and Family Communication a Priority
Patients and their families should always be at the center of the care process, and that means seamless provider-to-patient communication needs to be a top priority. Depending on the circumstance, communication with patients and their loved ones might include things like virtual appointments via video, text updates to family during a procedure, automated appointment reminders, and post-encounter surveys or follow-ups. These touch points are often vital for building patient-provider relationships and driving positive health outcomes.
There are many point solutions on the market for this kind of patient engagement, but your organization can’t achieve truly unified communication if clinician-to-clinician messaging is separate from clinician-to-patient messaging. Keeping all communication in the same platform ensures HIPAA compliance and makes it easy for care team members to engage with patients and their families as a regular course of business.
Benefits of Using One Communication Platform
Care Beyond the Walls of the Hospital
The amount of communication surrounding acute care patients is vast and understandably garners much of the focus, but patient care also happens in provider offices, ambulatory surgery centers, outpatient lab and diagnostic centers, and even patients’ homes. To meet the evolving needs and expectations of patients and providers, a platform needs to extend beyond the walls of the hospital.
If your technology can’t flexibly support care across all of these locations, it’s time to reconsider. That’s why using one platform for clinical communication, staff and provider scheduling, call/transfer/command center communication, after-hours call management, and patient engagement can fundamentally transform the way your staff collaborates on patient care. The right technology can quickly and effectively connect people—physicians, nurses, ancillary staff, patients, and patients’ families—without bounds.
Happier Providers, Happier Patients
Each piece of your communication puzzle works together to improve care delivery for patients, but provider satisfaction is just as crucial to high-quality patient care. Putting so many important pieces together in one platform enables doctors, nurses, and all other care team members to do their jobs without the roadblocks, delays, and frustrations that have been part of care coordination for far too long.
For patients, the care process becomes more interactive and accessible than ever before. No matter the issue, seeking care can be both frightening and confusing. It becomes infinitely worse when communication related to that care is tedious or difficult. From an outpatient perspective, when your patients know how to reach you and are confident that their outreach will be met with a timely answer, that’s a win for both sides. From an inpatient perspective, technology that facilitates efficient communication is a critical tool for clinicians trying to ensure positive health outcomes for their patients. Maybe it’s trite, but a healthy patient is a happy patient!
Finding the Right Communication Platform for Your Health System
Finding the right communication platform seems like a daunting task, but it doesn’t have to be. PerfectServe has been in the business of improving clinical workflows for over 25 years, and we can bring all of this experience to bear to help your organization implement an effective enterprise communication strategy.
Are you ready for real-time, unified communication? Contact us today.