Top Healthcare Trends in 2024
TABLE OF CONTENTS


If there’s one theme that might sum up the current state of healthcare, it’s the need for simplicity. But even though it’s at the top of many lists, it’s not the only priority.
By way of market evaluation, conversations with leaders, and analyses of C-suite reports, we’ve gathered some top trends and predictions we expect to hold significant weight in 2024.
Let’s jump straight into the trends, which are accompanied by tips for setting your health system up for success throughout the year.
Cost Savings
Maintaining financial sustainability amidst rising costs, reimbursement challenges, and shifting payment models is a persistent concern. It’s not surprising, then, that health systems are almost always looking for ways to trim costs.
There are many levers to pull, but some have the potential to generate the triple win of cost savings, workflow improvements, and greater simplicity all at once.
Some of these levers include consolidating your vendor footprint, finding fair and consistent price models for technology, and building a relationship with a scalable vendor who can advise on best practices for high-impact daily operations like care team collaboration.
With this focused approach on technology optimization, healthcare organizations can make life better (and less confusing) for clinicians while keeping costs in check.
Vendor Consolidation
Consolidation is so important, in fact, that it warrants even further discussion. Healthcare is in the middle of an aggressive digital transformation. Embracing this transformation is not a trend, but a necessity.
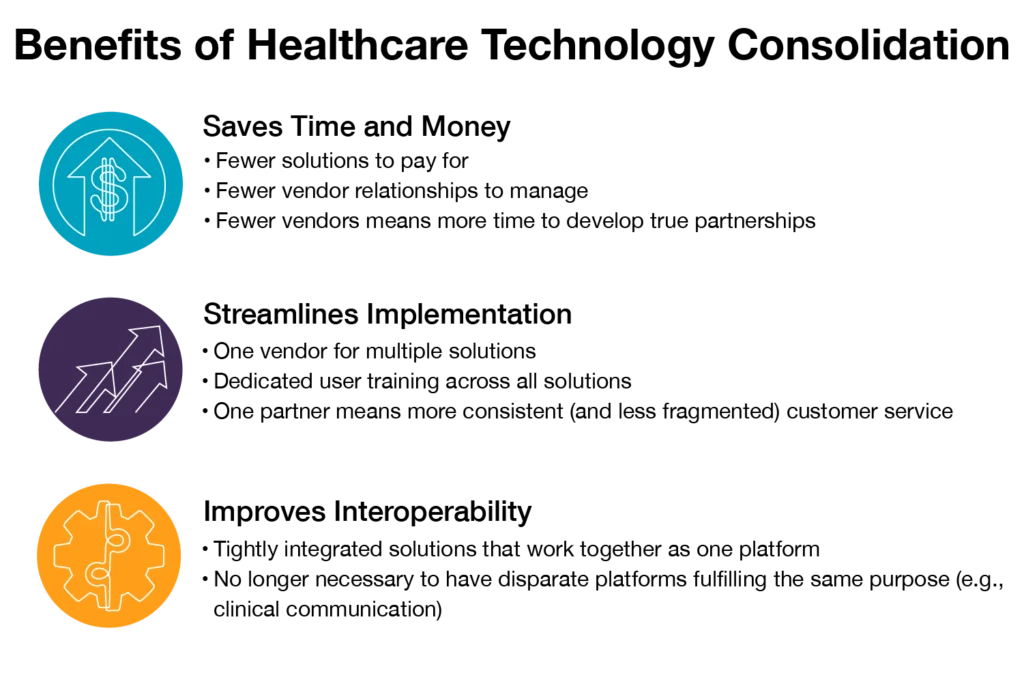
Consolidating healthcare technology is a hot topic because it can lead to everything from cost and time savings to a more streamlined implementation process to improved interoperability. There are many benefits:
Provider Wellness
The industry is still grappling with high levels of burnout, but the framing has shifted. Rather than talking only about combating burnout, many are focusing on promoting wellness.
Health systems are backing away from simply giving more days off. Instead, many are finding solutions that keep providers happy and healthy, making wellness a priority before burnout can take hold.
This trend is largely influenced by unbalanced schedules. A 2021 study revealed that over 52% of surveyed doctors “disagreed that their work schedule allowed work-life balance” (and a further 21% strongly disagreed).1
Pro tip: Find physician scheduling software that doesn’t just help with basic schedule management. To get at the factors that contribute to unbalanced schedules, you need scheduling tech that can optimize call shifts, promote shift equity, and take provider preferences into account.
Workforce Management Solutions
The industry also continues to face a growing shortage of healthcare workers, and it’s expected to worsen in the coming years.2
According to a 2023 report from Becker’s Healthcare, a main concern this year is navigating the workforce crisis and its connected challenges. The report claims the pandemic was a catalyst for many physicians leaving the field, “and many more plan to leave according to several industry surveys. Remaining physicians are often overburdened amid rising demand for care and the continued challenge of long-standing administrative burdens.”3
The focus this year is to address the shortage—at least partly—with workforce management tools that promote fairer schedules, optimize staffing models, grant deeper understanding with data and analytics, and boost resource utilization.
Patient Education
Research shows that strong patient-provider relationships tend to improve patient outcomes.4
Better patient education can impact hospital reimbursements, help to prevent chronic illness, reduce healthcare costs, boost clinician time savings, and improve the overall patient experience.
Health systems that understand the importance of patient education can use technology to improve communication and access to care while empowering patients to make informed decisions throughout their care journey.
Improving Clinical Communications
According to Miriam Halimi, Vice President of Clinical Informatics for PerfectServe, health systems that want to strengthen operations and achieve their growth goals need to make clinical communication one of their top priorities.
Here’s what some people don’t fully grasp: The work doesn’t just stop after deploying a healthcare communication platform. Optimizing care team communication in a way that consistently generates tangible outcomes—both for patients and clinicians—is an ongoing process that requires consistent attention.
Organizations interested in making communication a strength should find a vendor that can satisfy not just basic requirements, but also more advanced workflow opportunities that arise as the project evolves. A vendor shouldn’t just have the technology—they should have a wealth of experience and best practices to share.
In short, better communication should always be a trend. It’s something every care team member will benefit from.
Navigating these priorities requires a blend of strategic foresight, adaptability, and a continued commitment to delivering high-quality care. It’s essential to find a partner who can offer expertise, flexibility, and dedication to the strategic growth of your health system—one with the same healthcare trends in mind.
Sources
- Share of physicians whose work schedule leaves enough time for their personal and family life in the United States in 2021, Statista.com: https://shorturl.at/tENO3
- The Complexities of Physician Supply and Demand: Projections From 2019 to 2034, AAMC: https://www.aamc.org/media/54681/download
- Core Concerns for the Healthcare C-Suite: 2023 Quarter 3, Becker’s Heathcare: https://www.beckershospitalreview.com/
- Assessing the Longitudinal Impact of Physician-Patient Relationship on Functional Health, Annals of Family Medicine: https://www.annfammed.org/content/18/5/422