Live Event
Real solutions from experts who've moved the needle on burnout
Watch NowTABLE OF CONTENTS

Key Takeaways:
Back in 2008, only 9% of hospitals were using electronic health records (EHRs) to manage and protect patient records.1
Then came the Affordable Care Act, which brought a combination of incentives and mandates to spur adoption of EHRs. By 2014, fully 97% of all US hospitals were using EHRs.2
This rapid adoption was transformative for both providers and patients. But it was only the first step in a much longer effort to modernize care coordination because—contrary to what some EHR vendors might tell you—EHRs aren’t designed to do everything. And it’s okay to admit that.
As hospitals face growing pressure to increase patient throughput while also improving patient experience, the limitations of EHRs are becoming more obvious, especially when it comes to communication, care team collaboration, and operational efficiency.
If you’re serious about fixing these issues, you have to go beyond the native features of your EHR. And technology can still help you get there.
Let’s dive in to see how an updated strategy using the right tools can help you unlock more value from your EHR.
The original intent of EHR systems was to digitize medical records and all associated documentation. As these platforms have evolved over the years, innovation has been oriented around making this documentation easier, more accurate, and more valuable to clinicians. But EHR vendors have also broadened their focus to bring some built-in capabilities to other processes and systems.
“Now your EHR is the lab system of record, and the patient flow system,” says Ben Moore, Chief Innovation Officer at PerfectServe. “An EHR like Epic is building out functionality to support population health management and patient engagement—and they’re using AI in very compelling ways to do those things.”
EHRs have made great strides in consolidating select clinical workflows and systems so hospitals can run more efficiently. But to realize the full value of those workflow improvements, healthcare organizations need some additional infrastructure and capabilities that EHRs don’t supply.
Where EHR systems struggle
According to Ben, some of the EHR’s primary limitations revolve around resource scheduling and communication.
“When I say ‘resource,’ it could be scheduling a doctor, a nurse, or even an operating room theater or a piece of surgical equipment,” he says. “Almost every communication event inside a healthcare system is driven by a schedule.”
Scheduling for patients is one thing, and EHRs are better equipped to handle these tasks. But resource scheduling—and especially provider scheduling—is very specific and nuanced, and EHRs just don’t have the right tools to tackle it effectively. Every provider has their own scheduling preferences, and every hospital or clinic has constraints tied to equipment availability, compliance requirements, and revenue targets.
Plus, schedule changes often aren’t visible in the EHR in real time, which means time-sensitive messages won’t be received by the appropriate provider or staff member. This has direct implications for patient care.
Managing these variables efficiently requires a mix of intelligent routing and rules-based automation that isn’t available through EHRs, which are not natural-born communicators.
“Let’s say you [the patient] get a blood test, and one of your test results shows an abnormality that requires urgent intervention,” says Ben. “With Epic or another EHR, that notification goes to the physician’s inbox. But if they’re busy with a patient, or at their kid’s baseball game, and they left their phone in the car, that message could sit there for hours—and you won’t know you need immediate medical help.”
With the EHR at the center of the universe, the symptoms of broken scheduling coordination and care team communication are easy to find if you know where to look. Here are some clear signs your existing scheduling and communication methods are creating costly friction and delays in day-to-day operations:
Your real-time communication options are limited
EHRs don’t always integrate well with an organization’s other communication solutions, and their native messaging functions lack the logic and adaptive workflows needed to communicate in real time in a healthcare setting.
With limited routing features, a lack of escalation rules, and the inability to manage a cascading page system, EHRs—when trying to play the role of communicator—come with a number of constraints that can easily slow down hospital operations and provider responsiveness.
Providers are showing signs of burnout
Poor scheduling methods are often cited as a source of provider frustration. A scheduling solution that prioritizes equitable shift loads can dramatically impact provider morale and reduce rates of burnout.
One anesthesiology department switched to automated scheduling and saw a 55% increase in approvals for provider vacation requests, as well as a 30% increase in provider engagement scores within six months.
EHRs simply cannot handle the complexity and constant attention that provider schedules require. Why bother trying when purpose-built technology can do the trick?
Anything beyond local provider-to-provider communication is difficult
EHRs can facilitate provider-to-provider conversations and communication with some of the local care team. But communication beyond the EHR—and beyond the walls of the hospital—is limited and unreliable.
It isn’t all about patient care, either: EHRs don’t support a wide range of important operational communications, including weather alerts, construction notices, system downtime notices, and other messages that are critical to hospital staff, patients, and other external providers and partners.
Simply put, your healthcare communication platform can’t be walled off if you want operations to flow as smoothly as possible.
EHR platforms aren’t designed to integrate deeply or intuitively with the communication and scheduling tools that power your organization’s daily operations. That’s largely by design: EHR vendors have intentionally created closed ecosystems to try to lock customers into an EHR-first approach.
But EHRs themselves aren’t great communicators—and their poor interoperability with other communication tools only makes the issue worse. What health systems really need is a technology partner that supports integrations with all the clinical, IT, and telecom systems that make their facilities tick.
That collaborative approach leads to better results for your patients and your organization.
“At PerfectServe, we spend vast sums of our R&D budget to integrate with our competitors,” says Guillaume Castel, PerfectServe CEO. “Interoperability, for us, is not just a thing we do reluctantly. It is our strategy. Integrations are our strategy.”
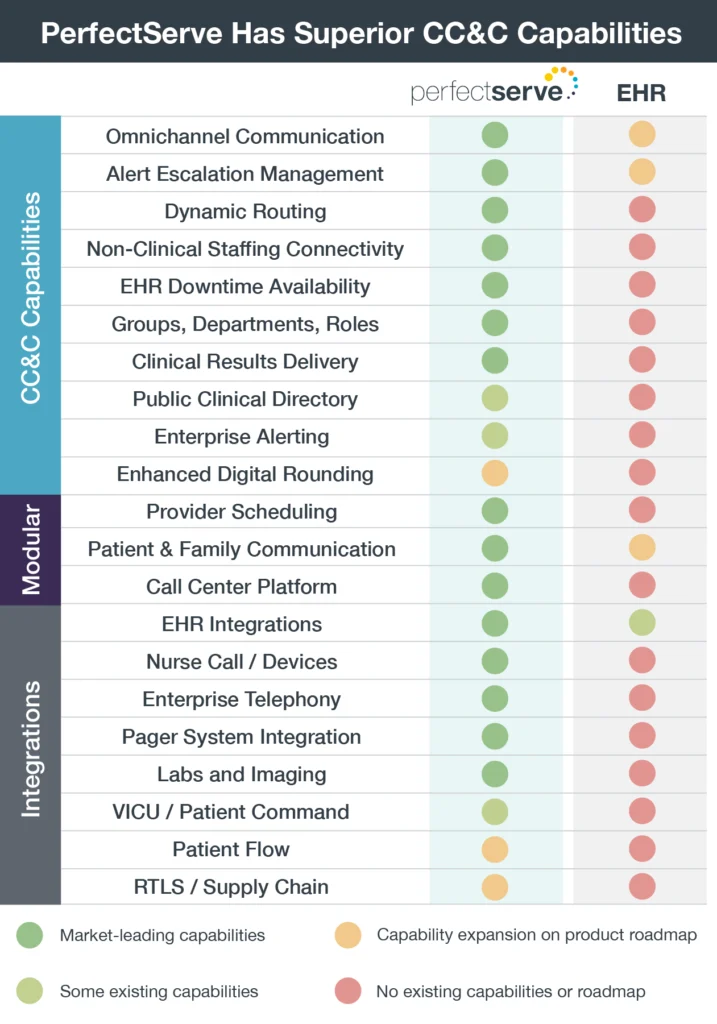
Here are three core features and functionalities that a clinical communication and collaboration (CC&C) platform can deliver when integrated with your EHR system:
The EHR’s communication struggles aren’t limited to its communication with outside systems. Even within a hospital or clinic, communication gaps create constant workflow delays that increase provider frustration and negatively affect patient care.
“The telephone systems, the nurse systems, the alerting systems—EHRs just don’t integrate well with [them],” says Ben.
PerfectServe has consolidated the capabilities of 14 different communication and workflow point solutions into its platform, which can then be integrated with Epic and many other EHRs to equip those systems with communication and care coordination capabilities that extend far beyond the walls of the hospital.
Proprietary technology like Dynamic Intelligent Routing (DIR) can route and escalate critical communications based on the real-time variables—date, time, urgency, service line—that are always changing in a healthcare setting.
This supercharges the EHR with new functionality for alert escalation management, clinical results delivery, and other omnichannel communications that happen outside the EHR, all of which benefit clinical workflows and overall patient care. In the urgent blood test example from earlier, PerfectServe’s DIR tracks and manages the delivery of that message to make sure it receives prompt attention.
“DIR monitors the message, and if it isn’t read or responded to within a certain timeframe, the platform escalates the message to the next on-call provider,” says Ben.
Provider scheduling is too variable to fit neatly into the one-size-fits-all EHR workflow. Instead, it requires modular, configurable processes to account for the many different rules and variables presented by provider preferences and individual patient cases.
Considering a tool that has advanced workflow-solving abilities to account for complex rules and preferences in provider scheduling. A surgeon, for example, may have preferences related to the clinical team he works with, and he may have strict requirements for when he needs to be out of the operating room to pick up his kids from school on Tuesdays.
EHRs have limited integration capabilities—which, as we discussed, are sometimes self-imposed by the EHR vendor—that can create costly workflow gaps during the care delivery process. PerfectServe addresses these gaps by supporting 250 different system integrations (and counting) to facilitate communications and other important clinical operations.
According to Ben, any given hospital may use 20 to 30 integrations to facilitate consistent communication across the care continuum.
“A lot of critical workflows need the ability to communicate outside of the EHR system,” he says. “Family members involved in the patient’s care don’t have the EHR app on their phone. The pharmacy down the street isn’t connected to the EHR. There are a lot of non-EHR users involved in the wellness of a patient, and they need communication channels that cross the barriers of the EHR system.”
EHRs are significant investments that get a lot of attention. And deservedly so. But it’s important to recognize that EHRs aren’t a one-to-one substitute for a platform built natively to handle complex communication and scheduling workflows.
When hospitals integrate a CC&C system with their EHR, they address the costly communication gaps and scheduling limitations inherent to EHR platforms and lay a foundation for greater operational efficiency and improved patient care. That means getting more value from your EHR investment and facilitating better outcomes for providers, patients, and your organization as a whole.
So no, we’re not gunning to become your next EHR vendor of choice. That’s never been the plan. But we do believe that EHRs and CC&C systems are better together.
Sources