Live Session
A Roadmap for Change Management Projects
Register NowTABLE OF CONTENTS
Simon Associates Management Consultants (SAMC) called 20 hospitals to assess the quality of the typical hospital call center experience. The callers claimed to be seeking help for their father who, they said, was diagnosed with prostate cancer. In most cases, the response was disappointing.
“Staffers hung up on us, told us to go to the website, or sent us to a contact who directed us somewhere else,” wrote Andrea Simon, Ph.D., CEO of SAMC, in an article for Becker’s Hospital Review. “As consumers, we were discouraged from ever going back to 90% of the hospitals.”1
SAMC’s results echoed broader call center statistics. Research from Salesforce found that 92% of all consumer interactions dissatisfied with their phone experience.2
Across industries, the call center is often the first stop on a consumer’s journey with a company. As a key entry point through an organization’s digital front door, one call can set the tone for the entire relationship. In healthcare, the role of the contact center is even more pivotal, since it serves as the critical communication bridge between patients and their care teams.
Health systems and technology companies are working both ends of the communication spectrum with efforts to improve both team collaboration and patient outreach. What’s often neglected is the call system in the middle, which leads to dropped calls, inefficient phone tag, transfer misfires, excessive on-hold times, and a missed opportunity to engage with patients and welcome them into the organization. The problem comes into clearer focus when you realize that losing just one patient to a competing health system due to an inefficient transfer process could mean missing out on up to $25,000 in potential patient revenue.
The solution to these problems is a fully integrated contact center, which seamlessly connects patients and providers, and solves the problems that have plagued health system call centers. The functionalities detailed in this guide are imperative building blocks to the ultimate solution.
Approaching the third decade of the 21st century, physicians should not still be required to retrieve messages like their predecessors did in the 1970s. Yet, despite rapid technology advancement throughout the rest of the hospital, many hospital call centers continue to operate with siloed legacy systems that don’t reliably connect with, or even operate independently from, essential hospital systems.
The challenges this presents are threefold:
1
Legacy systems can’t fully connect to the updated technology being used to improve workflow throughout the rest of the hospital (e.g. secure text messaging, on-call physician schedules, the CRM system, and the EHR), which means they can’t access patient reference data.
The Impact:
At the very least, the lack of integration prevents the hospitals from realizing the full benefits of the new technology. At worst, clinicians and staff are forced to retain old workflows alongside new ones, which creates frustration and increases the risk of medical errors. Disparate systems create numerous inefficiencies and require agents to manually look up phone extensions or pager numbers, leading to misdirected calls based on outdated call lists.
A lack of integration prevents the call center from functioning as a true contact hub that can deliver mass communications across the organization. Integration with secure text messaging and call schedules can allow contact center agents to activate code teams and send mass alerts during lockdowns, weather emergencies, and/or system outages.
Finally, agents who are inundated with inefficient switchboard tasks have little time to be proactive with patient care and engagement activities. Integration could transform agents from switchboard operators into true patient navigators.
2
Many call centers connect with providers via pagers, which rely on legacy, on-premise hardware at risk for outages and system failures. Pagers offer clinicians no way to distinguish an urgent message from a routine call, so precious time is often wasted waiting for physicians to respond to messages they may not realize are urgent. Then, if there is no response, operators have no way of knowing if the page was actually received, so their only recourse is to page the physician again.
The Impact:
Delays in message delivery and response may result in dangerous lapses in patient care. Furthermore, repeat pages and the lack of efficient message triage are key contributors to both physician burnout and operator fatigue. Frustrated patients who wait too long to receive call-backs ultimately may leave the health system to find more responsive care, resulting in lost revenue.
3
The legacy center system leaves numerous gaps where patient information may be compromised. Physicians may be forced to call in for messages from unsecured locations where PHI can be overheard during the conversation with the operator. Additionally, physicians frustrated with pagers have begun using unsecured SMS texting. Those who are aware of the HIPAA risks inherent in this practice often engage in workarounds that attempt to obscure patient identity, e.g. “Mrs. X in room 2235 needs pain medication.” Such practices have led to incorrect identification of patients, which can lead to serious lapses in patient care.
The Impact:
The mean financial penalty for a HIPAA violation in 2018 was more than $2.5 million, so protecting PHI is a critical concern for hospital administration.5 The workaround is even worse and exposes hospitals to tremendous risk if a dangerous error results from patient misidentification.
Integration with other hospital systems can transform the traditional call center into a health system’s communication command center and patient engagement center. The first step is to ensure the contact center platform is integrated with the following key clinical systems:
Connection to a secure messaging platform allows agents to relay messages as texts or traditional voice messages. When the contact center is connected to a HIPAA-compliant secure communication platform, operators can send messages to clinicians with complete patient details. Clinicians can receive full messages instantly on their smartphones and can respond to callers immediately.
The entire process layer of phoning back into the call center can be eliminated. This alone enables patients to receive call-backs from their physicians within minutes instead of an hour or more. Agents can also see when text messages have been delivered and read, so uncertainty and repeat pages are no longer an issue.
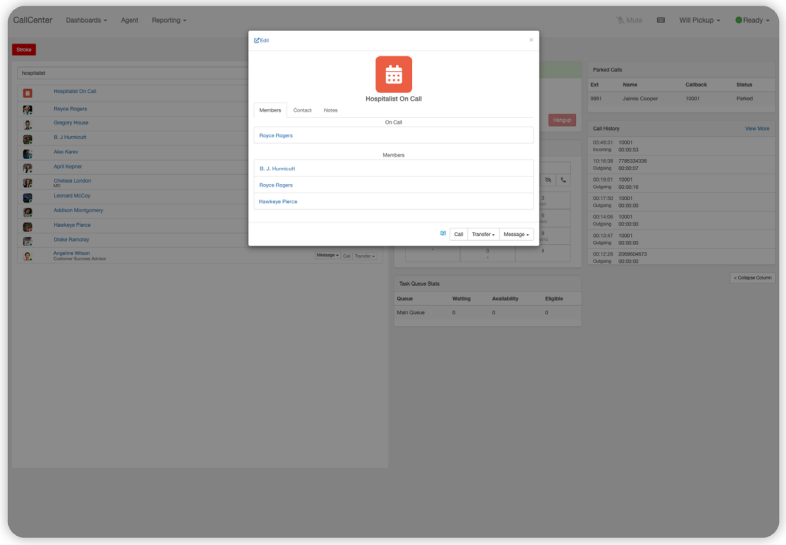
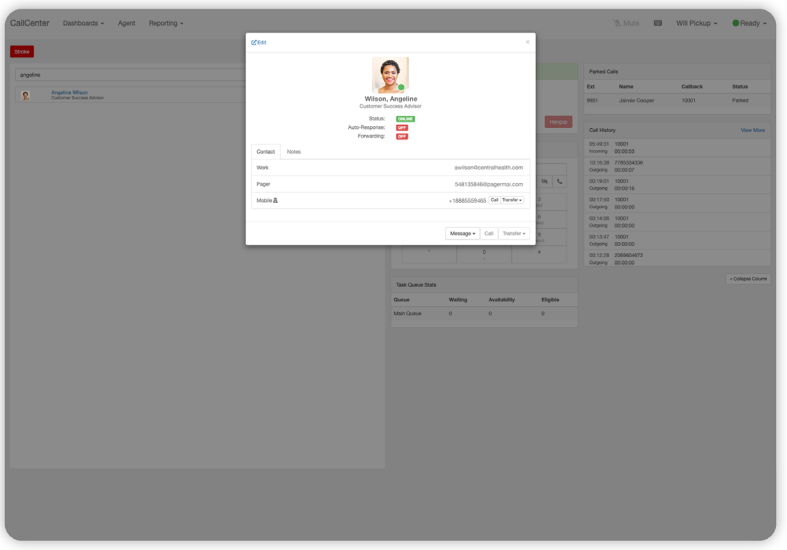
An easy search in a unified directory should pull up any clinician in the hospital or health system, along with their preferred contact preferences. A simple click should connect the agent to the clinician via text, call, or page, depending on their preferred method. Directory integration enables fast connection to hospital departments, unit desks, ambulatory practices, pharmacies, and more. An ideal, flexible system allows agents to search for any care team member by name, department, or role across all locations within an organization.
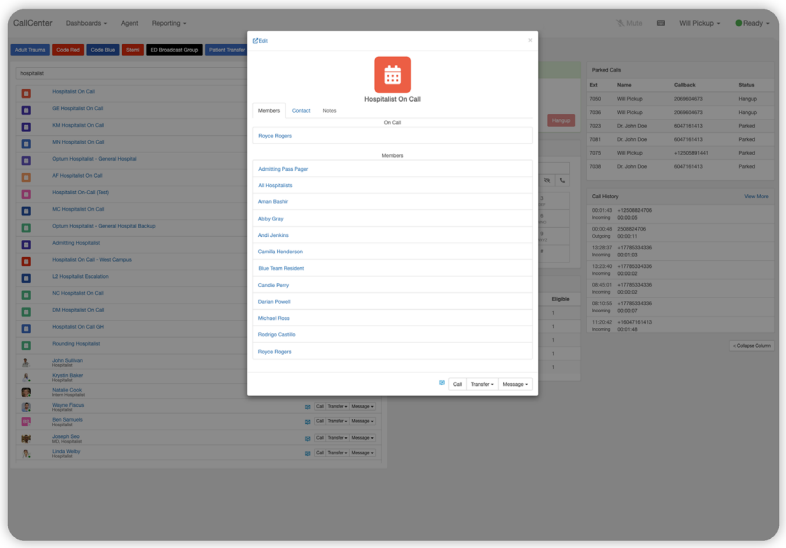
Integration with a hospital’s scheduling software allows operators to reliably route calls to the correct clinicians. Agents should have a single, updated view of the schedule across all departments and locations. Since this is digitized, paper- based systems can be eliminated and schedules can reflect real-time updates.
Operators no longer need to know a name to locate the appropriate on-call clinician when they can search the clinical directory by role for “Hospitalist On Call” or “ED Charge Nurse.” With scheduling integration, time is never wasted on misdirected calls or texts.
Once the directory and schedules are integrated, agents can message groups to easily execute code calls and clinical activations, such as engaging STEMI, trauma, or stroke teams. Contact center agents should be able to click one button to activate the desired team, with visibility into which clinicians have seen, read, and responded to the activation.
Consoles with EHR access can pull up a patient’s care team and inpatient information to direct calls and messages to the correct team member. Calls and messages can be routed to the patient’s on-call nurse, physician, hospital unit clerk, a member of the care team, or directly to the patient’s room. Secure text messages can be sent to individuals on the care team or to the care team as a whole. Messages can include attachments with patient details, such as their room number, as an easy reference for the recipient.
When a contact center platform is integrated into an existing customer relationship management (CRM) system, the CRM can use caller ID matching to pull up the customer record at the start of the call. This allows for instant identification of the patient and immediate access to call history, which facilitates faster resolution and dramatically improves the customer experience. Follow-up notes can also be pushed back into the CRM to document the call.
Connection to patient flow systems that manage care teams and bed allocations helps ensure that resources and teams are adequately enabled for inbound patients.
For a complete solution, an integrated contact center should be able to direct dial any type of phone, such as PBXs, hospital extensions, other locations within the network, and patient rooms.
While pager replacement is often the ultimate goal for a hospital or health system, an integrated contact center platform should be able to send messages to existing pagers. This allows clinicians and response teams to retain functionality they’re accustomed to while improving the reliability of message delivery.
Integrating the contact center module with key hospital systems solves the problems of a legacy call center platform by enabling a critical functionality: two-way communication. Here’s what two-way communication should look like for a hospital system:
With siloed systems, operators lose all visibility once a call leaves the call center platform and is “parked.” The operator has no way of knowing and, more importantly, no opportunity to intervene, if the physician fails to respond or if the caller gets stranded on hold. With legacy systems, physicians have to call in to confirm receipt of the message or to be redirected to a waiting caller.
A fully integrated contact center platform enables two-way communication between the contact center and clinicians. It can accommodate warm or blind transfers and provide full visibility into physicians’ availability, current contact information, and preferred contact methods (phone, text message, or even legacy pager).
This is what “park and page” should look like when it’s working properly. It helps contact center agents keep track of calls from beginning to end, with full visibility into the call and physician message and response lifecycles. If a patient waits too long on hold, an agent can be alerted and intercede. The system can operate first-in, first-out by default, but it should also be customizable based on the needs of the organization. With various call queues, agents can jump in and pick up any call regardless of location.
The following additional contact center conveniences should also be included:
With the contact center in control of the full life cycle of each call, agents should no longer have to spend time fielding multiple calls from the same patient or resorting to overhead pages for group alerting or to track down physicians.
Messages from the contact center should follow delivery and escalation rules and reach physicians according to their preferred contact method—text, phone call, or pager number. If a physician is tied up in a patient encounter, the message can be routed automatically based on established routing rules that ensure critical messages are never missed. Routing can follow rules based on on-call schedules, role, and seniority.
Today’s platforms should offer contact center operators the functionality to broadcast critical messages to the entire user base or individual broadcast groups. Emergency alerts, such as a hurricane or flood warnings, and backup instructions during EMR outages can be activated instantly from the contact center. Since messages can be sent directly to users according to their communication preferences, disruptive overhead announcements are no longer needed.
By putting mass notifications into the solution, the hospital or health system can reduce its vendor footprint, eliminating the licensing costs and workflow inefficiencies associated with managing a completely different platform for mass alerts. The system should also provide tracking to document when messages were received and when key personnel responded—a feature that’s critical for demonstrating due diligence for compliance.
With a PFC platform, agents can become care navigators, not just switchboard operators, to serve as a critical first touchpoint in the organization’s digital front door. With built-in intelligence to flag patient survey responses, agents can receive notifications to triage and forward to practitioners as needed. The system should also help agents manage everything from patient phone interactions and text messages to appointment reminders and post- discharge follow-up. Tasks that may have required manual intervention from call center agents in the past can now be automated and tracked through the PFC platform.
A Kentico study confirmed that patients are looking for more follow-up and engagement from their health care providers. In fact, 69% of the patients surveyed found value in texted appointment reminders and procedure guidelines.7 Text messages can be easily automated to free up time for more meaningful patient engagement, which helps facilitate better care, optimize the patient experience, enhance patient satisfaction, and even improve HCAHPS scores. With the ability to manage calls, text messages, and pages, today’s contact center can become an omnichannel hub of communication.
Cloud technology can dramatically increase the functionality and reliability of a traditional on- premise call center, transforming it into a modernized contact center. Agents on a cloud-based contact center platform can access their dashboards and take calls from any location, empowering them to manage call volume with incredible flexibility, even 24 hours a day.
This is ideal for multi-site health systems, as well as merged and acquired hospitals. The contact center can be unified without physically moving the agents. For example, a healthcare system can leverage overhead operator and reception resources from any location and provide them virtual call queues from a busier location.
Cloud technology is also scalable and can adjust seamlessly to higher call volume. Lines are virtually limitless compared to a traditional finite system. This is how integrated, cloud-based systems can reserve a line for a call until it is completely resolved. The cloud also allows for rapid implementation and easy deployment of new features and functionalities.
At some point, health systems on cloud-based communication platforms typically experience an event that reaffirms the decision to move to an off-premise critical communication ecosystem.
Something unexpected may take down the rest of the organization’s technology systems, but the cloud-based contact center platform keeps the entire health system informed during the execution of a recovery plan.
A recent Deloitte Global Contact Center Survey described integrated analytics as “the holy grail” for most organizations working to merge multiple systems. Advanced analytics topped the list of capabilities organizations were planning to invest in related to the patient experience and/or contact center(s).8
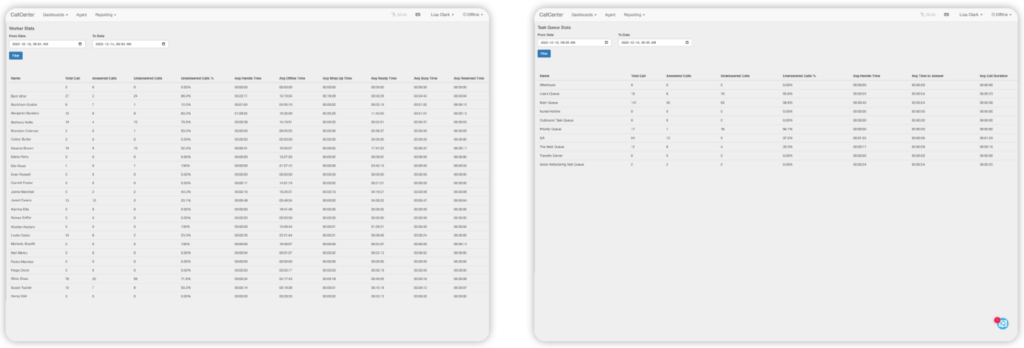
In healthcare, the integrated contact center platform offers full visibility across numerous metrics, such as average wait time and call duration, to provide accurate data for analysis and improvement. Calls can be reviewed from initiation to outcome to determine where delays occurred, confirm call resolutions, and even listen to recordings. Managers and administrators can sort data by agent, location, date—whatever provides the best information for uncovering opportunities for success and improvement. Supervisors can also use the dashboard to manage agents and queues.
The fully integrated contact center is ideal for all aspects of healthcare call center management. By enabling seamless omnichannel connection between patients and their providers, the fully integrated contact center platform can fix a broken link in the hospital communication chain.
When administrative load is decreased and the call center is integrated with key hospital systems, it is transformed into a comprehensive contact command center. This upgrade brings agents into the patient engagement ecosystem and empowers them to deliver a frictionless patient experience as a critical component of the digital front door. The less time agents spend navigating siloed systems and working around legacy technology, the more they can engage patients and facilitate higher quality care.
The integrated contact center platform should be designed, deployed, and optimized alongside a clinical communication platform. The following best practices ensure optimal success.
When deployed alongside a comprehensive clinical communication platform, a cloud-based contact center solution becomes part of a powerful, interconnected communication ecosystem capable of driving powerful outcomes in many different areas.
PerfectServe has spent more than 25 years improving clinical workflows for thousands of healthcare organizations. Challenges and goals differ from one organization to the next, so there’s no such thing as a one-size-fits-all solution, but there are a number of demonstrable outcomes achieved by individual PerfectServe customers that showcase the proven and repeatable possibilities afforded by unified care team communication and collaboration:
Financial Performance
Patient Outcomes
Clinician Experience
By making the contact center an integral part of a broader clinical communication blueprint, your organization can drive better patient and clinician experiences, reduce costs, and more judiciously utilize the care team’s time and effort.

