Connect Care Teams and Provide
Unparalleled Value for the Hospital

Providers
Protect physicians’ time and improve speed to care with a comprehensive clinical communication solution.
- Prevent unnecessary disruptions
- Reduce communication cycle times
- Accommodate personal preferences
- Reach the right clinician every time via text, call, or video
- Facilitate instant notification of critical results, consult requests, and more


Technology Teams
Consolidate and integrate communication platforms while improving the nurse and provider experience.
- HIPAA-compliant, SOC 2 certified, and recognized as a “Cybersecurity Transparent” pioneer by Censinet and KLAS
- Cloud-based to reduce burden on IT
- Replace pagers, texting, operator console and DECT phones to reduce total cost of ownership
- Integrate with EHRs, scheduling, nurse call, middleware, LIS, DECT phones, and operator consoles to improve clinical workflows

Operations
Improve hospital metrics with an outcomes-based approach to communication.
- Efficient care team collaboration can improve patient outcomes and reduce length of stay
- Automate tedious manual workflows
- Improve clinician satisfaction and HCAHPS scores
- Consolidate clinical systems and reduce overhead costs
Healthcare Communication Made Easy
Customized Algorithms
We compile and maintain all the workflow rules, call schedules, and contact preferences for every workgroup, practice, and care team member.
Targeted Coordination
Never worry about figuring out who’s on call. With guided workflows, Dynamic Intelligent Routing reliably connects you to the right person who can take action at that moment.
Patient-Centered Access
All you need to know is the patient’s name. PerfectServe instantly shows and connects you to the team members caring for that patient at that time.
Multimodal
PerfectServe supports and unifies all devices (smartphones, web browsers, landline phones, VoIP devices, pagers) and modalities (text, call, video).
Responsive Escalation
PerfectServe knows when the recipient has read a message. Unread messages automatically escalate based on defined protocols to ensure no communication is missed.
Advanced Search
Easily connect with any member on the PerfectServe platform inside your organization and across your healthcare ecosystem.
Drive System-Wide Outcomes
13 sec
Reduced Time to Contact On-Call Providers from Eight Minutes
82%
Reduction in Time Spent Managing Schedules
73%
Improvement on Rapid Response Times
+2.3 pts
Increase in HCAHPS Hospital Rating
42%
Improvement in Average Acknowledgement Time for Critical Lab Results
+$680k
Annual Savings After Replacing Pagers and Answering Services
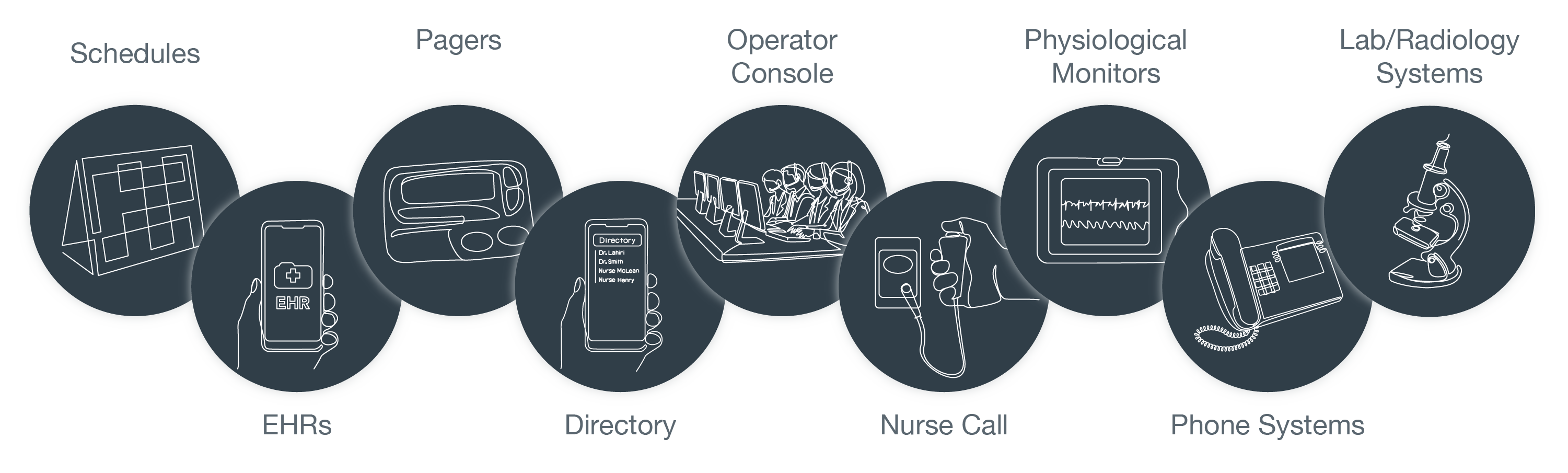
Integrate with Clinical and IT Platforms
Improve speed to care by connecting your healthcare communication platform with key clinical, IT, and telecom systems.



 Magic Quadrant
Magic Quadrant






