What is a Clinical Communication and Collaboration Platform?
TABLE OF CONTENTS
Healthcare is a jargon- and acronym-heavy industry, often to the point of confusion. As an example, most can intuitively deduce what the term “clinical communication” means, but if someone inquired about which “CC&C” solution your hospital uses, would you even understand what they’re asking? Probably not, and you’re not alone. Let’s fix that by breaking it down.
Secure Messaging, Integrations, and Better Workflows, Oh My!
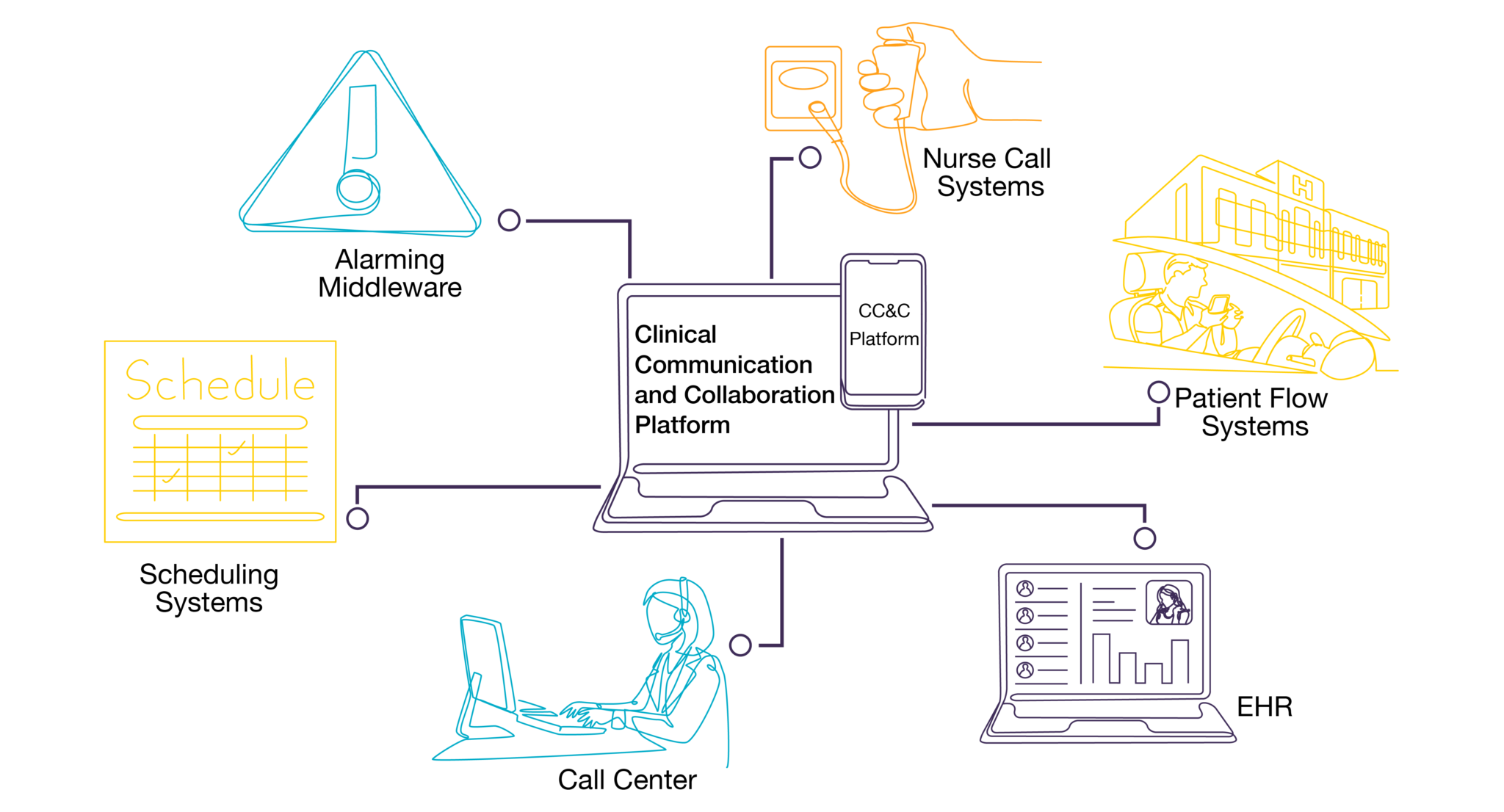
Clinical communication and collaboration (CC&C) platforms are secure messaging solutions that integrate with other clinical systems to enhance workflows for physicians, nurses, and other care team members using an application accessible from smartphones and desktops. These platforms evolved from basic secure messaging solutions, which came to market with a strict focus on HIPAA-compliant texting. CC&C solutions support a much broader range of capabilities and now stand as powerful vehicles for integrated messaging and data transmission.
Secure messaging systems traditionally provided HIPAA-compliant texting and voice communication capabilities to safely transmit patient information, but as technology and the healthcare industry at large have evolved, so have the scope and proficiency of these solutions. A CC&C platform goes further by ingesting data from the EHR to provide clinicians with their patient lists, current care team members, detailed patient information, and more. Providers can also message other care team members and see patient context—date of birth, location, and other critical information—right on their mobile device. This evolution has streamlined the way providers communicate with one another while yielding new opportunities to speed up the care delivery process.
Some CC&C platforms can also integrate with clinical scheduling solutions to provide an instant view of clinician availability and who’s on call. Other key integrations include nurse call to improve patient response times, call center to incorporate an important hub of patient interaction into the broader communication ecosystem, hospital phones to maintain familiar communication paths (like extensions for certain departments), and much more. These more complex workflows enhance provider communication, provide insight into improving response times for things like sepsis or STEMI activations, improve coordination for admissions and discharges, and decrease feelings of provider burnout by removing friction from common clinical activities.
By reducing the time it takes to coordinate care—and creating better communication workflows for providers overall—CC&C systems allow clinicians to spend more time with patients, which can improve everything from job satisfaction to HCAHPS scores to patient safety, outcomes, and throughput.
What Do Clinical Communication and Collaboration Platforms Do?
- HIPAA-compliant text messaging and voice communication, which includes the ability to send videos and images
- Message/call escalation and routing based on users’ role or availability
- Ability to view and update schedules from your smartphone
- Instant notification of critical lab results, orders, admissions, discharges, critical alarms, and time-sensitive team alerts (STEMI, sepsis, etc.)
- Ability to call back to a patient’s room from your smartphone when the nurse call button has been activated
- Send emergency broadcast messages related to weather, an active shooter, coding, or other events when expedited mass communication is necessary
- Facilitate message auditing with time and date stamps to see when all communications are sent, delivered, and read
Common Integrations
CC&C platforms most commonly integrate with scheduling systems, nurse call, patient flow systems, alarming middleware, call center, and EHRs.
As further advancements are made, additional integrations will surface to facilitate even more clinical workflows. With more than 200 supported integrations, PerfectServe’s CC&C platform is capable of unifying communications and streamlining care coordination for healthcare organizations of all sizes. Learn more about the benefits of these integrations here.
Choosing the Right Clinical Collaboration Software
Choosing the right vendor can be overwhelming, but it’s best to focus on specific use cases to identify which platform will most significantly improve communication and care team collaboration for your physicians, nurses, and other staff. When the care team is equipped with a CC&C platform that supports powerful communication workflows and a wide range of clinical integrations, downstream benefits with improved speed to care are almost a certainty.
To learn more about what we can do for your health system, schedule a demo or give us a call today. You can also read our in-depth guide to selecting a clinical communication platform or explore our customer success stories to see how other hospitals and health systems have benefited from using PerfectServe.