Physician Engagement: What It Is and Why It’s Important
TABLE OF CONTENTS
In healthcare, the impact of workforce engagement has similarities with other industries such as productivity, turnover, and financial performance. However, physician engagement significantly impacts the health, safety, and well-being of the patient experience and outcomes. The good news is clinical communication and collaboration solutions can address those common denominators while improving the quadruple aims of patient outcomes, experience, cost reduction, and clinician satisfaction.
Why is Physician Engagement Important?
Physician engagement is critical for a successful patient care experience. When physicians feel a lack of association, it manifests itself in ways ranging from physician burnout to a poor patient experience.
Engaged physicians are 26% more productive than those less engaged, adding an average of $460,000 in additional patient revenue per year.
Physician employment does not automatically equal engagement. Communication and collaboration skills are a must-have regardless of the number of employed physicians. High levels of physician engagement have been correlated to increased productivity, generate more referrals, expand influence amongst peers and medical staff, and drive organizational strategy and change. When medical practitioners are engaged, patients and the local economy reap the benefits.
“Patient experience impacts revenues, referrals, adherence, safety, and the credibility of an institution with the community.” – Forbes
What is Physician Engagement?
Engaged physicians take greater care of their patients, reduce medical costs, and are more efficient than their unengaged counterparts. The Health Care Advisory Board states that creating organizational alignment is one of the most challenging initiatives, but the most crucial to success—impacting cost, quality, and experience initiatives.
PHYSICIAN ENGAGEMENT DEFINITION
A strategy that focuses on streamlining communication, building relationships, and aligning physicians with the values, vision and mission of their organization and with other healthcare stakeholders to continuously improve care and the patient experience.
BENEFITS OF PHYSICIAN ENGAGEMENT
• Reduced referral leakage.
• Increased in-network referrals.
• Higher engagement of patient population.
• Improved patient care delivery.
• Enriched physician development and performance.
• Decreased burnout and turnover rates.
Effective engagement strategies require a multifaceted approach. One that includes retention, clinical and cultural fit, onboarding, benefits, leadership development, formal recognition, and physician burnout.
Measuring Physician Engagement
Surveys
Consistently measure and invite physicians to share their needs and challenges to gauge physician sentiment and identify gaps within care teams and workflows.
Run monthly engagement surveys for insights into how physicians perceive your organization and its services. Using that information, closely examine the factors that contribute positively or negatively to engagement and create a plan to improve physician’s everyday experience.
Scorecards
Help physicians understand what is expected of them in a transparent way while measuring productivity and performance metrics.
“We feel transparency is extremely important in order to change behavior. The scorecard gives a comparison of provider to provider within the same specialty. And then it’s a provider to their individual practice. And then it’s that provider to the network.”
Travis Turner, Mary Washington Healthcare
Dashboards & Reporting
Employ platforms that enable your organization to visualize sufficient, real-time data. This drives organizational initiatives and empowers physicians to have the autonomy to course-correct quality to improve care delivery.
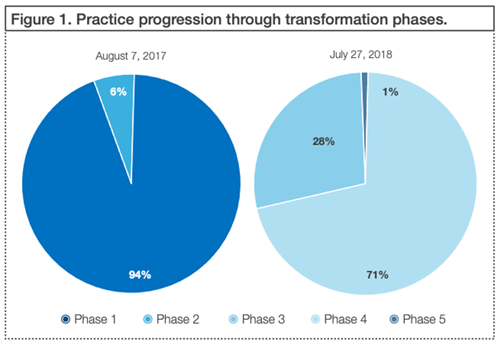
Develop an in-house practice transformation dashboard to show overall movement of your practice through the phases of your organizational initiatives. Here’s an example of a dashboard used in the special report Practice Transformation Analytics Dashboard for Clinician Engagement, published by Annals of Family Medicine.
Accountability Tools
Implementing a solution that provides your organization and physicians to practice accountability enables both personal, peer-to-peer, and clinical autonomy. Solutions that use read receipts, automatic escalations, and self-managed scheduling can foster opportunities for meaningful dialogue and potentially reduce burnout.
There are hundreds of ways to slice your data. Look back to your guiding questions to determine the most important KPIs for your organization’s unique goals and priorities.
Mid-Atlantic Nephrology Associates reduced operational costs by over $9k by modernizing practice communication for a network of more than 52 facilities, 50 providers, and 1,700 patients.
Improving Physician Engagement
Provide Pathways to Influence
Create physician-led channels to the executive suite to share their voice in decision-making. This reframes the narrative of physicians from employees to partnerships, creating a forum for open dialogue between executives and physicians.
Invite physicians to join leadership in roundtable discussions. This fosters an environment where physicians know their voice is heard, helps identify leadership opportunities, and shows commitment to invest in formal and informal opportunities to develop physician leaders and influencers.
Launch a ‘North-Star’ Initiative
Workflows and systemic factors are universal and aren’t limited to one group of care providers. By demonstrating the intent of how multiple initiatives interconnect, it streamlines the number of things physicians are asked to do on top of their patient care routines. As an example, Figure 1 shows how the factors and behaviors that build a safer culture, drive positive outcomes.
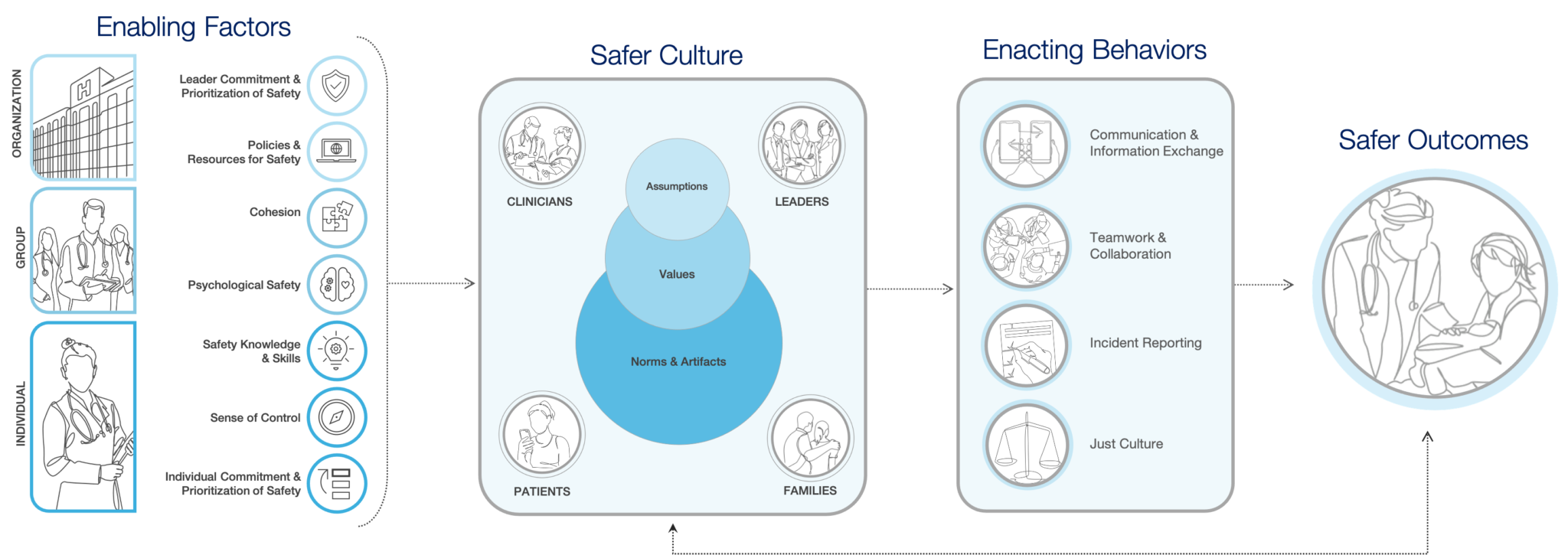
Note: Figure adapted from Bisbey et al. (2019)
Create a Data Strategy
Data should be applied and not simply collected. An effective way to drive physician engagement is to build a comprehensive data strategy that improves transparency and helps physicians understand the objectives their organization is driving.
North Memorial Healthcare adopted an enterprise data warehouse (EDW) with visualization capabilities to enable physicians to get near real-time answers to their clinical quality improvement questions. The physicians could then see how their decisions affected length of stay (LOS) and how specific changes in clinical processes would improve LOS. By accessing the data, it was easier to convince physicians to make the needed changes.
Form Leadership Development Programs
Physician relationships with staff, background, future planning, and training differ among hospital leaders. This creates challenges in how rapidly physicians are able to respond to marketplace and regulatory change. Adopt intentional leadership development programs for physicians who are both formal and informal leaders.
• Hold annual leadership summits with executives and the c-suite.
• Establish physician champions to present peer-selected awards.
• Kick off meetings with peer-recognized moments of excellence.
• Form topics of interest or medical specialty groups for collaboration.
How Does Technology Improve Physician Engagement?
Physicians are trained to be patient care providers, not data-entry administrators.
Physician engagement in technology is critical for the future of care delivery, and physicians are looking for solutions that streamline clinical practice, allow more face-to-face time with patients and improve outcomes. The secret is to improving physician engagement in technology adoption is by illustrating why the technology is needed. Take time to involve physicians in the selection and implementation process, and provide data to show how it benefits them and the patients.
Achieving more balance in providers day-to-day is possible with the right technology solution. When looking for a clinical communication and collaboration platform, look for solutions that have considered end-users in the build of the user interface and capabilities. Does it have interoperability across technology, and the capabilities to streamline workflows to increase operational efficiency? Look at the processes it takes and how the platform integrates with EHR systems to improve the medical practitioner’s experience.
In a high stress environment, recognizing physician needs can empower them to implement new technologies. As a result, this can improve satisfaction levels, assist in making better care decisions, and support patient engagement and satisfaction levels.